THE ORIGIN OF THE SARS CORONA VIRUS ( COVID-19 )
THE VIRUS
On 30 December 2019, three bronchoalveolar lavage samples were collected from a patient
with pneumonia of unknown etiology – a surveillance definition established following the
SARS outbreak of 2002-2003 – in Wuhan Jinyintan Hospital. Real-time PCR (RT-PCR) assays
on these samples were positive for pan-Betacoronavirus. Using Illumina and nanopore
sequencing, the whole genome sequences of the virus were acquired. Bioinformatic
analyses indicated that the virus had features typical of the coronavirus family and belonged
to the Betacoronavirus 2B lineage. Alignment of the full-length genome sequence of the
COVID-19 virus and other available genomes of Betacoronavirus showed the closest
relationship was with the bat SARS-like coronavirus strain BatCov RaTG13, identity 96%.
Virus isolation was conducted with various cell lines, such as human airway epithelial cells,
Vero E6, and Huh-7. Cytopathic effects (CPE) were observed 96 hours after inoculation.
Typical crown-like particles were observed under transmission electron microscope (TEM)
with negative staining. The cellular infectivity of the isolated viruses could be completely
neutralized by the sera collected from convalescent patients. Transgenic human ACE2 mice
and Rhesus monkey intranasally challenged by this virus isolate induced multifocal
pneumonia with interstitial hyperplasia. The COVID-19 virus was subsequently detected
and isolated in the lung and intestinal tissues of the challenged animals.
Whole genome sequencing analysis of 104 strains of the COVID-19 virus isolated from
patients in different localities with symptom onset between the end of December 2019 and
mid-February 2020 showed 99.9% homology, without significant mutation.
NOTE
- COVID-19 virus is referred to as 2019-nCoV, the interim virus name WHO announced early in the
outbreak.
2. COVID-19 is referred to throughout as novel coronavirus pneumonia or
NCP, the term by which COVID-19 is most widely known in the People’s Republic of China.
Post-mortem samples from a 50-year old male patient from Wuhan were taken from the
lung, liver, and heart. Histological examination showed bilateral diffuse alveolar damage
with cellular fibromyxoid exudates. The lung showed evident desquamation of
pneumocytes and hyaline membrane formation, indicating acute respiratory distress
syndrome (ARDS). Lung tissue also displayed cellular and fibromyxoid exudation,
desquamation of pneumocytes and pulmonary oedema. Interstitial mononuclear
inflammatory infiltrates, dominated by lymphocytes, were seen in both lungs.
Multinucleated syncytial cells with atypical enlarged pneumocytes characterized by large
nuclei, amphophilic granular cytoplasm, and prominent nucleoli were identified in the intra-alveolar spaces, showing viral cytopathic-like changes. No obvious intranuclear or intracytoplasmic viral inclusions were identified.
THE OUTBREAK
As of 20 February 2020, a cumulative total of 75,465 COVID-19 cases were reported in
China. Reported cases are based on the National Reporting System (NRS) between the 6
National and Provincial Health Commissions. The NRS issues daily reports of newly
recorded confirmed cases, deaths, suspected cases, and contacts. A daily report is provided
by each province at 0300hr in which they report cases from the previous day.
The epidemic curves presented in Figures 2 and 3 are generated using China’s National
Infectious Disease Information System (IDIS), which requires each COVID-19 case to be
reported electronically by the responsible doctor as soon as a case has been diagnosed. It
includes cases that are reported as asymptomatic and data are updated in real time.
Individual case reporting forms are downloaded after 2400hr daily.
DEMOGRAPHIC CHARACTERISTICS
Among 55,924 laboratory confirmed cases reported as of 20 February 2020, the median age
is 51 years (range 2 days-100 years old; IQR 39-63 years old) with the majority of cases
(77.8%) aged between 30–69 years. Among reported cases, 51.1% are male, 77.0% are from
Hubei and 21.6% are farmers or laborers by occupation.
ZOONOTIC ORIGINS
COVID-19 is a zoonotic virus. From phylogenetics analyses undertaken with available full
genome sequences, bats appear to be the reservoir of COVID-19 virus, but the intermediate
host(s) has not yet been identified. However, three important areas of work are already
underway in China to inform our understanding of the zoonotic origin of this outbreak.
These include early investigations of cases with symptom onset in Wuhan throughout
December 2019, environmental sampling from the Huanan Wholesale Seafood Market and
other area markets, and the collection of detailed records on the source and type of wildlife
species sold at the Huanan market and the destination of those animals after the market
was closed.
ROUTES OF TRANSMISSION
COVID-19 is transmitted via droplets and fomites during close unprotected contact between
an infector and infectee. Airborne spread has not been reported for COVID-19 and it is not
believed to be a major driver of transmission based on available evidence; however, it can
be envisaged if certain aerosol-generating procedures are conducted in health care facilities.
Fecal shedding has been demonstrated from some patients, and viable virus has been
identified in a limited number of case reports. However, the fecal-oral route does not
appear to be a driver of COVID-19 transmission; its role and significance for COVID-19
remains to be determined. Viral shedding is discussed in the Technical Findings (Annex C).
HOUSEHOLD TRANSMISSION
In China, human-to-human transmission of the COVID-19 virus is largely occurring in
families. The Joint Mission received detailed information from the investigation of clusters
and some household transmission studies, which are ongoing in a number of Provinces.
Among 344 clusters involving 1308 cases (out of a total 1836 cases reported) in Guangdong
Province and Sichuan Province, most clusters (78%-85%) have occurred in families.
Household transmission studies are currently underway, but preliminary studies ongoing in
Guangdong estimate the secondary attack rate in households ranges from 3-10%.
CONTACT TRACING
China has a policy of meticulous case and contact identification for COVID-19. For example,
in Wuhan more than 1800 teams of epidemiologists, with a minimum of 5 people/team, are
tracing tens of thousands of contacts a day. Contact follow up is painstaking, with a high
percentage of identified close contacts completing medical observation. Between 1% and
5% of contacts were subsequently laboratory confirmed cases of COVID-19, depending on
location. For example:
• As of 17 February, in Shenzhen City, among 2842 identified close contacts, 2842
(100%) were traced and 2240 (79%) have completed medical observation. Among
the close contacts, 88 (3.1%) were found to be infected with COVID-19.9
• As of 17 February, in Sichuan Province, among 25493 identified close contacts,
25347 (99%) were traced and 23178 (91%) have completed medical observation.
Among the close contacts, 0.9% were found to be infected with COVID-19.
• As of 20 February, in Guangdong Province, among 9939 identified close contacts,
9939 (100%) were traced and 7765 (78%) have completed medical observation.
Among the close contacts, 479 (4.8%) were found to be infected with COVID-19.
Testing at fever clinics and from routine ILI/SARI surveillance
The Joint Mission systematically enquired about testing for COVID-19 from routine
respiratory disease surveillance systems to explore if COVID-19 is circulating more broadly
and undetected in the community in China. These systems could include RT-PCR testing of
COVID-19 virus in influenza-like-illness (ILI) and severe acute respiratory infection (SARI)
surveillance systems, as well as testing of results among all visitors to fever clinics.
In Wuhan, COVID-19 testing of ILI samples (20 per week) in November and December 2019
and in the first two weeks of January 2020 found no positive results in the 2019 samples, 1
adult positive in the first week of January, and 3 adults positive in the second week of
January; all children tested were negative for COVID-19 although a number were positive for
influenza. In Guangdong, from 1-14 January, only 1 of more than 15000 ILI/SARI samples
tested positive for the COVID-19 virus. In one hospital in Beijing, there were no COVID-19
positive samples among 1910 collected from 28 January 2019 to 13 February 2020. In a
hospital in Shenzhen, 0/40 ILI samples were positive for COVID-19.
Within the fever clinics in Guangdong, the percentage of samples that tested positive for the
COVID-19 virus has decreased over time from a peak of 0.47% positive on 30 January to
0.02% on 16 February. Overall in Guangdong, 0.14% of approximately 320,000 fever clinic
screenings were positive for COVID-19.
SUSCEPTIBILITY
As COVID-19 is a newly identified pathogen, there is no known pre-existing immunity in
humans. Based on the epidemiologic characteristics observed so far in China, everyone is
assumed to be susceptible, although there may be risk factors increasing susceptibility to
infection. This requires further study, as well as to know whether there is neutralising
immunity after infection.
CHILDREN
Data on individuals aged 18 years old and under suggest that there is a relatively low attack
rate in this age group (2.4% of all reported cases). Within Wuhan, among testing of ILI
samples, no children were positive in November and December of 2019 and in the first two
weeks of January 2020. From available data, and in the absence of results from serologic
studies, it is not possible to determine the extent of infection among children, what role
children play in transmission, whether children are less susceptible or if they present
differently clinically (i.e. generally milder presentations). The Joint Mission learned that
infected children have largely been identified through contact tracing in households of
adults. Of note, people interviewed by the Joint Mission Team could not recall episodes in
which transmission occurred from a child to an adult.
THE SIGNS, SYMPTOMS , DISEASE PROGRESSION AND SEVERITY
Symptoms of COVID-19 are non-specific and the disease presentation can range from no symptoms (asymptomatic) to severe pneumonia and death. As of 20 February 2020 and 12 based on 55924 laboratory confirmed cases, typical signs and symptoms include: fever (87.9%), dry cough (67.7%), fatigue (38.1%), sputum production (33.4%), shortness of breath (18.6%), sore throat (13.9%), headache (13.6%), myalgia or arthralgia (14.8%), chills (11.4%), nausea or vomiting (5.0%), nasal congestion (4.8%), diarrhea (3.7%), and hemoptysis (0.9%), and conjunctival congestion (0.8%). People with COVID-19 generally develop signs and symptoms, including mild respiratory symptoms and fever, on an average of 5-6 days after infection (mean incubation period 5-6 days, range 1-14 days). Most people infected with COVID-19 virus have mild disease and recover. Approximately 80% of laboratory confirmed patients have had mild to moderate disease, which includes non-pneumonia and pneumonia cases, 13.8% have severe disease (dyspnea, respiratory frequency ≥30/minute, blood oxygen saturation ≤93%, PaO2/FiO2 ratio <300, and/or lung infiltrates >50% of the lung field within 24-48 hours) and 6.1% are critical (respiratory failure, septic shock, and/or multiple organ dysfunction/failure). Asymptomatic infection has been reported, but the majority of the relatively rare cases who are asymptomatic on the date of identification/report went on to develop disease. The proportion of truly asymptomatic infections is unclear but appears to be relatively rare and does not appear to be a major driver of transmission. Individuals at highest risk for severe disease and death include people aged over 60 years and those with underlying conditions such as hypertension, diabetes, cardiovascular disease, chronic respiratory disease and cancer. Disease in children appears to be relatively rare and mild with approximately 2.4% of the total reported cases reported amongst individuals aged under 19 years. A very small proportion of those aged under 19 years have developed severe (2.5%) or critical disease (0.2%).
As of 20 February, 2114 of the 55,924 laboratory confirmed cases have died (crude fatality
ratio [CFR2] 3.8%) (note: at least some of whom were identified using a case definition that
included pulmonary disease). The overall CFR varies by location and intensity of
transmission (i.e. 5.8% in Wuhan vs. 0.7% in other areas in China). In China, the overall CFR
was higher in the early stages of the outbreak (17.3% for cases with symptom onset from 1-
10 January) and has reduced over time to 0.7% for patients with symptom onset after 1
February (Figure 4). The Joint Mission noted that the standard of care has evolved over the
course of the outbreak.
Mortality increases with age, with the highest mortality among people over 80 years of age
(CFR 21.9%). The CFR is higher among males compared to females (4.7% vs. 2.8%). By
occupation, patients who reported being retirees had the highest CFR at 8.9%. While
patients who reported no comorbid conditions had a CFR of 1.4%, patients with comorbid
conditions had much higher rates: 13.2% for those with cardiovascular disease, 9.2% for
diabetes, 8.4% for hypertension, 8.0% for chronic respiratory disease, and 7.6% for cancer.
The Battle of Unseen
More than 6000 positive cases of covid19 were reported in california in a single day as per the reports.
Though many preventive measures have been taken up by the state authorities since the outbreak of virus but it is hard to tell who and who may not the vector of the contagious virus. It has been few days since some states reopened their economies and just in a matter of time, huge numbers are being reported each single day.
A person could be looking very normal even if he/she has this virus. This is because the symptoms may take time. This could be upto several days when the symptoms start showing up and in that meantime, that person would have meet up so many people, including family, friends, colleagues and many more. So the spread of this virus is fast and exponential.
The numbers that are being reported worldwide everyday are from the people that have been screened and tested. If the testing capacity is increased, it is quite expected that the figures may show up in a horrible range.
Besides precautions and safety protocols, Governments are also suggesting their public to avoid panic situations. It is a psychological factor that when someone look at the figures reported, it brings fear inside the head and this fear synergistically affect the overall condition.
It was being heard previously that almost a big percentage of the world’s population would be affected by this virus. Those who get affected should stay home and get themselves quarantined. Let them stay isolated for sometime and when they become negative for virus, they shall live normally.
Figures may keep rising for an indefinite period of time. It is hard to tell when would this pandemic gets to an end. World is demanding the vaccine. Scientists are struggling at their best. Even, many doctors are requesting the people who have got well from the infection to donate their blood for the plasma. This plasma is helpful in keeping the patients to go into severe conditions.
Source: http://www.health.com
What is Dexamethasone? New Research Says Steroid Can Reduce Mortality Ratio in Covid-19 Patients With Severe Conditions
The drug has been found potent in reducing mortality ratio by 17% in coronavirus patients with severly ill conditions but some doctors have still objections over its reported benefits.
It has been nearly six months since corona virus a.k.a Covid-19 has been gripping the world and in this shot period of time, multiple medications—namely hydroxychloroquine ( Commonly used antimalarial drug and recently had its emergency use authorization revoked by the FDA) and remdesivir, an antiviral drug currently in the lead for proven, albeit modest benefits in treatment)—have been found as “game-changer” in the treatment.
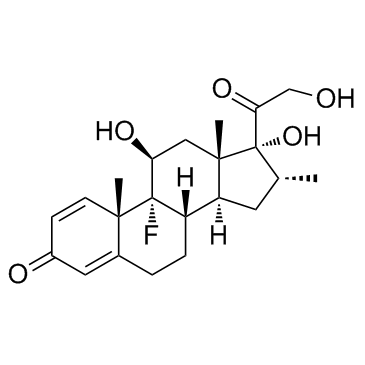
We have recently got an add on in the tray of medicines that are presently given in the treatment of corona virus. Pharmacologically, Its a corticosteroidal molecule, commonly known as Dexamethasone. This information has been received from a statement released on Tuesday from chief investigators who conducted clinical trial in uk regarding the effectiveness of dexamethasone in severly ill or hospitalized covid-19 patients who require oxygen because of their respiratory systems being compromised due to virus. Dexamethasone has been found potent upto the extent that scientists are pondering to recognize this molecule as a standard in the treatment against covid-19.
This could be because of the mechanism of action of steroids or their nature, being anti inflammatory. Thus, reducing the inflammation inside the respiratory system paving the way for oxygen supply and the patient gets able to breathe smoothly. It is admirable to have such effects against covid-19 but there is a need of more trials and research as whether using steroids could be beneficial in long run? Because historically, It has been observed that using steroids may lead to many cardiac, renal and hepatic dysfunctions or disorders.
It must be kept at the front that dexamethasone is not the only drug currently being used. Besides, other forementioned drugs are also on the list including azithromycin which is a very commonly used antiobiotic. Being respiratorily compromised, one may lead to cardiac arrests, shock conditions and many severe conditions as well. Drugs have their therapeutic windows and index which means that every drug has its potency within a particular range of dose. Once it is crossed, It could lead to toxic effects. Just for the sake of an example, i would like to include that a very commonly used pain killer in our societies in paracetamol ( Brand Name: Panadol ). It comes in 500mg tablet normally. But it could be harmful for the human body if the blood levels reaches upto certain amount.
Reference: http://www.health.com
